Introduction
The intricate relationship between testosterone levels and urinary health in men has garnered significant attention in recent urological research. Testosterone deficiency, a condition affecting a notable percentage of American men, has been linked to various health issues, including an increased risk of kidney stone formation. This article delves into the specific patterns of urine sediment crystallization observed in testosterone-deficient men and discusses the implications for stone formation risk, with a focus on urological health tailored to the American male population.
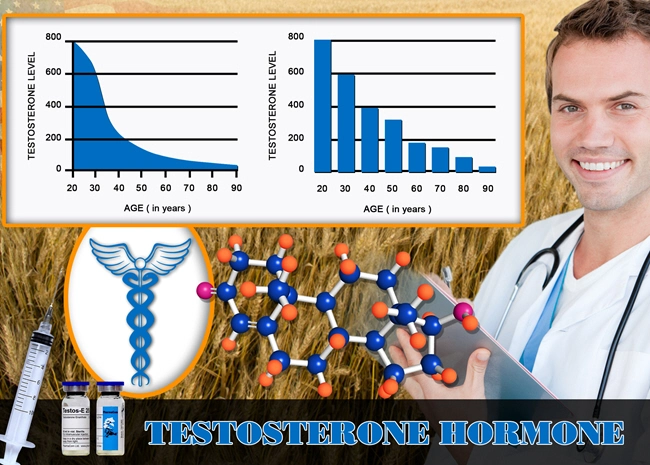
Understanding Testosterone Deficiency
Testosterone deficiency, also known as hypogonadism, occurs when the body does not produce enough testosterone, a crucial hormone responsible for male physical characteristics and overall health. In the United States, this condition affects approximately 2.1% to 12.8% of men, with prevalence increasing with age. Symptoms can range from reduced libido and erectile dysfunction to fatigue and increased body fat. Recent studies have begun to explore the less obvious effects of testosterone deficiency, including its impact on urinary health and kidney function.
Urine Sediment Crystallization and Kidney Stones
Kidney stones are a common urological disorder, characterized by the formation of hard deposits made of minerals and salts within the kidneys. The crystallization of urine sediment is a critical step in the formation of these stones. Research has shown that testosterone levels can influence the composition and concentration of urine, thereby affecting the crystallization process. In testosterone-deficient men, alterations in urine pH and the concentration of stone-forming substances like calcium, oxalate, and uric acid can lead to increased crystallization and, subsequently, a higher risk of stone formation.
Patterns Observed in Testosterone-Deficient Men
Studies focusing on American men have identified distinct patterns in urine sediment crystallization among those with testosterone deficiency. These men often exhibit higher levels of calcium oxalate crystals, which are the most common type of kidney stone. Additionally, the presence of uric acid crystals, another prevalent stone type, is also more frequent in this population. The increased crystallization is attributed to changes in urine composition, including a more acidic pH and elevated levels of stone-forming substances, which are influenced by the hormonal imbalance.
Implications for Stone Formation Risk
The observed patterns of urine sediment crystallization in testosterone-deficient men have significant implications for their risk of developing kidney stones. The increased presence of calcium oxalate and uric acid crystals suggests a heightened risk, necessitating targeted prevention and management strategies. American men with testosterone deficiency should be aware of this increased risk and consider regular urological screenings to monitor their kidney health.
Management and Prevention Strategies
Managing and preventing kidney stones in testosterone-deficient men involves a multifaceted approach. Increasing fluid intake to dilute urine and reduce the concentration of stone-forming substances is a primary recommendation. Dietary modifications, such as reducing salt and animal protein intake, can also help manage urine composition. In some cases, testosterone replacement therapy may be considered to address the hormonal imbalance and potentially mitigate the risk of stone formation. However, this should be approached cautiously and under the guidance of a healthcare professional, as it can have various side effects and implications.
Conclusion
The link between testosterone deficiency and increased kidney stone formation risk through altered urine sediment crystallization patterns is a critical area of focus for urological health in American men. Understanding these patterns and their implications can lead to more effective prevention and management strategies, ultimately improving the quality of life for those affected. As research continues to evolve, it is essential for men with testosterone deficiency to stay informed and proactive about their urinary health.
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- Alpha1-Adrenoreceptor Density, Testosterone, and LUTS Severity in American Men: Current Insights [Last Updated On: March 3rd, 2025] [Originally Added On: March 3rd, 2025]
- Ultrastructural Implications of Testosterone Deficiency on Bladder Muscle: Electron Microscopy Insights [Last Updated On: March 7th, 2025] [Originally Added On: March 7th, 2025]
- Managing Urethral Epithelial Atrophy: Androgen Deficiency and Hormone Replacement Therapy Explained [Last Updated On: March 8th, 2025] [Originally Added On: March 8th, 2025]
- Testosterone's Impact on Prostate Stroma: Collagen and Elastin Dynamics Explored in Study [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- Unveiling the Role of Prostatic Acid Phosphatase in Monitoring Androgen Activity During Testosterone Replacement Therapy in Men [Last Updated On: March 10th, 2025] [Originally Added On: March 10th, 2025]
- Androgen-Dependent Regulation of Phosphodiesterase Type 5 in Prostatic Tissue: Implications for Male Urological Health [Last Updated On: March 10th, 2025] [Originally Added On: March 10th, 2025]
- Unveiling the Impact of Hormone Replacement on Pelvic Floor Electromyographic Activity in Hypogonadal Men [Last Updated On: March 12th, 2025] [Originally Added On: March 12th, 2025]
- Exploring Post-Void Residual Volume Changes in Men with Low Testosterone: A Longitudinal Study on Hormone Replacement Therapy [Last Updated On: March 13th, 2025] [Originally Added On: March 13th, 2025]
- Exploring Urinary Proteomics in Androgen-Deficient Men: Unveiling New Biomarkers for Lower Urinary Tract Dysfunction [Last Updated On: March 15th, 2025] [Originally Added On: March 15th, 2025]
- Metabolomic Analysis of Prostatic Fluid in Testosterone-Deficient Men: Urological Insights [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Urinary Flow Cytometry Insights into Hypogonadism and Testosterone Therapy Effects [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Testosterone Deficiency Impacts Mitochondrial Function in Bladder Smooth Muscle: Urological Insights [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Androgen-Regulated Genes in Urothelium: HRT Impact and Urological Health Insights [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Prostatic Inflammation in Hypogonadal Men: Histopathology and TRT Benefits [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Vesicourethral Reflux in Hypogonadal Men: Bladder Neck Dysfunction and Hormonal Impact [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Testosterone Deficiency's Impact on Lower Urinary Tract Autonomic Innervation: A Quantitative Analysis [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Aging Men's Prostate Health: Aromatase Activity, Testosterone Therapy, and BPH Risks [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- TRT's Impact on Prostate Health: Assessing Blood Flow with Color Doppler Ultrasonography [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Prostatic Neuroendocrine Cells in Androgen-Deficient Men: Analysis and HRT Response [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Neural Density in Detrusor Muscle of Hypogonadal Men: Clinical Insights for American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Testosterone Therapy Impact on PSA Kinetics and Prostate Health Monitoring Protocols [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Testosterone Therapy's Impact on Prostatic Hyperplasia in Hypogonadal Men: Morphometric Insights [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Urodynamic Insights into Detrusor Overactivity and Testosterone Deficiency in Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- UPP in Hypogonadal Men: Pre- and Post-ART Insights for Urologists [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- TRT's Impact on Prostate Health Monitored by Transrectal Shear Wave Elastography [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- TRT's Impact on Prostatic Arterial Flow: Doppler Ultrasonography Insights for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Ultrasonographic BWT and Urodynamics in Men with Late-Onset Hypogonadism: Clinical Insights [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- DSD in Androgen-Deficient Men: Prevalence, Urodynamics, and Management Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Testosterone Deficiency and Bladder Function in American Men: Insights from AUM [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Testosterone's Influence on Bladder ECM: GAGs, PGs, and Men's Urological Health [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- TRT Enhances Urinary Flow in Hypogonadal Men: Uroflowmetric and Hormonal Insights [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Testosterone Therapy's Impact on Non-Bacterial Prostatitis in Hypogonadal Men: Inflammatory Mediators [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Androgen Deficiency Impact on Urinary Flow: Urodynamic Analysis and Hormonal Insights [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- TRT's Impact on Micturition Parameters in American Males with Hypogonadism [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Androgen Receptor Distribution in Lower Urinary Tract of Hypogonadal Men: Immunohistochemical Insights [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Urinary Exosomal miRNAs: Biomarkers for Monitoring LUTS Treatment in Hypogonadal American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Prostatic Calcifications in Hypogonadal Men: Prevalence, Composition, and LUTS Association [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Prostatic Urothelial Metaplasia in Hypogonadism: Prevalence and Testosterone Therapy Impact [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- TRT and Prostate Health: Growth Factors and Hyperplasia in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Postvoid Dribbling in Testosterone-Deficient Men: Insights and Hormone Therapy Solutions [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Testosterone's Impact on Prostate Gap Junction Proteins and Health Implications [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Testosterone Therapy's Impact on Prostate Cell Proliferation: A Histomorphometric Study [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypogonadism's Impact on Bladder Neck Collagen and Urodynamic Function in Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- LOH Impact on Bladder Compliance in American Men: Urodynamic and Hormonal Insights [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Nocturnal Polyuria in Testosterone-Deficient Men: Mechanisms and Hormone Therapy Benefits [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone Replacement Therapy Improves Bladder Function in Hypogonadal Men: A Cystometric Study [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Androgen Therapy Modulates Apoptotic Index in Hypogonadal Men's Prostatic Epithelium [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Androgen Deficiency Impacts Bladder Function via Contractile Protein Expression in Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Neurogenic Bladder in Hypogonadal Men: Urodynamics, Hormones, and Clinical Management [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone Deficiency Effects on Prostatic Secretions: Biochemical Analysis and Health Implications [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Neurophysiological Impact of Testosterone on Bladder Sensory Afferents in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone's Impact on Detrusor Oxygenation in American Men with Androgen Deficiency [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Urethral Sphincter EMG Changes in Hypogonadal Men Post-Testosterone Therapy: Urological Insights [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone Therapy and PIN Incidence in Hypogonadal Men: Surveillance and Management [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- PSMA Expression Analysis in Androgen-Deficient American Men Before and After ART [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- TRT's Impact on Prostatic Smooth Muscle in American Men: Electron Microscopy Insights [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Testosterone Fluctuations in TRT and Maximum Urinary Flow Rate Variability in Hypogonadal Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Mapping Prostatic Stromal ARs in American Men with LUTS: Therapeutic and Diagnostic Insights [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Testosterone Deficiency and Bladder Sensation: QST Insights Before and After HRT [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Estrogen's Role in LUTS: Prostatic Stromal Aromatase Activity in Aging Men [Last Updated On: April 3rd, 2025] [Originally Added On: April 3rd, 2025]
- Testosterone Deficiency and Bladder Function: Impact and Improvement via HRT [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- TRT Enhances Urethral Function in Hypogonadal Men: UPP Topography Study [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- 3D Ultrasonography: Monitoring Prostate Health in Men on Testosterone Therapy [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Testosterone Deficiency and Bladder Wall Fibrosis: Impact and HRT Benefits in American Men [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Diurnal Testosterone Variations and LUTS in Hypogonadal Men: Insights and Implications [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Testosterone Deficiency and Bladder Function: Myofibroblast Insights for American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Revolutionizing Urology: Assessing Androgen Receptor Sensitivity in Prostatic Tissue [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Prostatic Elastography: Monitoring Prostate Health in Men on Testosterone Therapy [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Testosterone Therapy Benefits for Hypogonadal Men with Prostatitis-like Symptoms [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Testosterone Therapy's Impact on Overactive Bladder in Androgen-Deficient American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Power Doppler Ultrasonography Enhances TRT Monitoring in American Males' Urological Health [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- TRT's Impact on Autophagy in Prostatic Cells of Hypogonadal American Males [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Intraprostatic Hormone Fluctuations Before and During Testosterone Replacement Therapy in Men [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]