Video Link: https://vimeo.com/275725072
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Video Link: https://vimeo.com/279256045
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
How to Understand and Deal with Cirrhosis
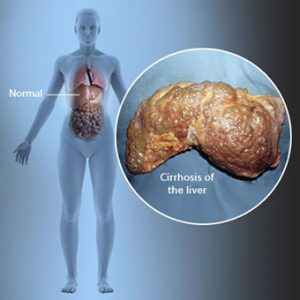
Cirrhosis. It is the most common liver disease. And one of the most dreaded and feared liver diseases. Cirrhosis is defined as the scarring of the liver tissue and is caused by chronic, long-standing liver disease.
 Cirrhosis is particularly insidious since it can progress for years, even decades before it is detected.
Cirrhosis is particularly insidious since it can progress for years, even decades before it is detected.
In fact, researchers have concluded that up to 80% of the liver can suffer damage before showing any symptoms.
And often, when it is detected, the damage is irreversible. If cirrhosis continues on its path of destruction, the result may be liver cancer.
Under the lens of a microscope, hepatocytes (liver cells) show a massive amount of scarring. The damage formula is simple: the more scarring you see, the more damage the liver has suffered.
Here’s an analogy to keep in mind. If you slash your hand while chopping vegetables, you will suffer a deep wound. Eventually, a protective scar will form on your hand. Regrettably, scars on the skin are permanent and generally do not dissolve over time.
Liver scarring is called fibrosis. Fibrosis occurs as a reaction to damage to the liver that kills liver cells. These dead cells are replaced by regenerating cells that cause the liver to harden.
Fibrosis usually occurs over extended periods of time. When the liver is under assault from a broad range of reasons (see below), the cells can become inflamed, since the liver is trying to battle the infection or recover from an injury.
If the damage continues unabated, the liver cells will scar and replace healthy liver cells. If the scarring is not stopped, it may lead to cirrhosis. If the injury is still not halted, eventually all the liver cells will harden. This is the final stage of cirrhosis and may lead to liver cancer.
Why is the Liver So Important?
Before we continue, a brief review of the liver’s vital, life-saving functions is in order. The liver is responsible for processing (metabolizing) almost everything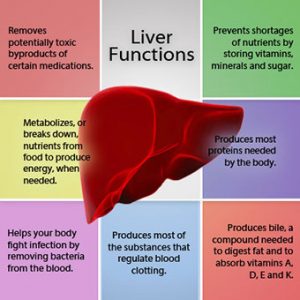 that goes down our throat, that we inhale into our lungs, and absorb through our skin: the foods we eat, the liquids we drink, the pills we swallow, and environmental pollutants that we come into contact with daily.
that goes down our throat, that we inhale into our lungs, and absorb through our skin: the foods we eat, the liquids we drink, the pills we swallow, and environmental pollutants that we come into contact with daily.
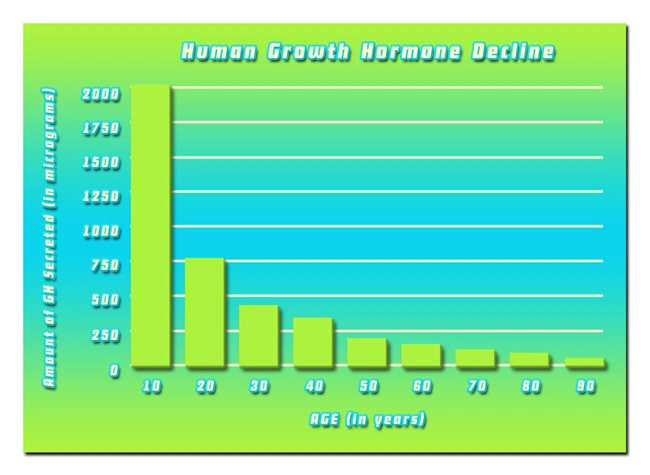
The digestive system sends nutrient-rich blood through the liver to begin its journey of delivering nutrients throughout the body. Also, the liver metabolizes many of our hormones.
The liver is also responsible for clotting your blood, producing cholesterol, detoxifying the body, providing protein, making chemicals to battle viruses and bacteria, blocking substances that promote the growth of cancer, and helping to fine-tune the body’s immune system.
This is just beginning to scratch the surface of the liver's importance. The liver is a real workhorse; it performs hundreds of tasks daily. Hopefully, you can see how vital the liver is. When its function is impaired, you are impaired. When your liver quits, you quit. It’s that simple.
The problem is that some of these substances we ingest (alcohol, environmental chemicals, and certain drugs) are toxic to the liver.
If the bombardment of toxins continues non-stop, the liver can become overloaded, and eventually begin to shut down.
What Causes Cirrhosis?
The first step in dealing with cirrhosis is determining what is causing the disease. Here are the main reasons:
- Chronic hepatitis B or C
- Long-term heavy alcohol abuse
- Non-alcoholic fatty liver disease (NAFLD). When this condition progresses, it may develop into non-alcoholic steatohepatitis (NASH).
- Primary biliary cirrhosis
- Primary sclerosing cholangitis
- Gallstones
- Genetic diseases
The Signs and Symptoms of Cirrhosis
As scar tissue in the liver increases, the pressure in the liver can grow. This development is called “portal pressures” since pressure builds in the portal vein.
When this pressure rises to a level higher than 35 millimeters of mercury, the condition is called portal hypertension.
This causes fluid to accumulate resulting in several symptoms:
- Ascites, which is the buildup of fluid in the abdomen. This can cause weight gain and an expanding waistline. If the condition gets worse, it may need draining by a medical professional. This removal process is called paracentesis. In advanced cases, this may need to be performed weekly.
- Edema. This is an accumulation of fluid in the legs and ankles. The key here is to remember that there are many other causes of edema (heart disease, kidney disease). Therefore, a link between the liver and edema must be established by a medical professional.
- Jaundice.
- Lack of appetite.
- Weight-loss.
- Muscle and joint aches.
- Muscle weakness.
- Chronic fatigue.
- Excessive bleeding or bruising.
- Dark urine.
- Cognitive problems. This is serious, extremely serious. Fatigue, insomnia, memory issues, and an inability to focus may be tied directly to liver problems. If your liver is not functioning optimally, toxins can accumulate and lower the oxygen level in the blood. Eventually, these toxins may travel to the brain. Ammonia levels can increase which and may lead to a condition called hepatic encephalopathy which results in confusion and fatigue.
- Incessant itching. This happens when the liver is unable to process bilirubin (a brownish yellow substance found in bile, produced when the liver breaks down old red blood cells). The accumulation of bilirubin leaks into the skin and may result in maddening itching.
The Stages of Fibrosis
There are several steps of liver fibrosis. If a blood test detects liver abnormalities, often a liver biopsy is performed. This biopsy is done by inserting a needle into the liver and removing a tiny sample of liver tissue.
This allows doctors to asses the degree of liver damage and determines the stage of liver fibrosis. The scale of fibrosis runs from 0 to 4. Here is the breakdown:
- Stage 0 = no fibrosis.
- Stage 1 = portal area expansion.
- Stage 2 = fibrosis is expanding from the portal area and making a few bridges between portal areas.
- Stage 3 = an increasing number of fibrosis bridges advancing toward the center areas of the liver
- Stage 4 = cirrhosis
Other Organs are Affected by a Beaten-up Liver
Remember, the liver performs the lion’s share of work in so many areas. If the liver is compromised and unable to purify the blood, that added burden is passed to the kidneys.
 The problem with that? The kidneys are overworked due to the added workload from the colon as a result of a damaged liver.
The problem with that? The kidneys are overworked due to the added workload from the colon as a result of a damaged liver.
When the kidneys are weakened, the bladder is stressed, and the toxin explosion continues. It resembles a merry-go-round from hell.
If all of this weren’t bad enough, the adrenal glands, the heart, and the stomach are also at increased risk due to cirrhosis.
What You Can Do to Make Your Liver Happy
If you don’t have cirrhosis, or any liver damage, great! Keep reading and learn how to keep your liver healthy.
If you are suffering from liver damage that may lead to cirrhosis, or if you have cirrhosis, these are steps you need to take immediately to give your liver a fighting chance.
You Are What You Eat
Athletes know that you can’t out-train sloppy eating habits. Bodybuilders know that abdominal muscles (“abs”) are made in the kitchen. Dieters understand the price that is paid for excessive cheating.
There’s no getting around it. The phrase “you are what you eat” may be a cliché, but it’s true. And this goes double for those with cirrhosis.
Make sure your eating plan is jam-packed with liver-friendly foods: beets, apples, citrus fruits, squash, carrots, broccoli, cabbage, cauliflower, zucchini, and watercress.
watercress.
Cruciferous vegetables are crucial since they are loaded with glucosinolates, compounds which assist enzyme production in the liver. In turn, these enzymes sweep out toxins and carcinogens, which lowers cancer risk.
Dark, leafy greens are a vital addition to your diet. They contain chlorophylls (the green coloring matter of leaves and plants) which help get rid of environmental toxins.
Protein is crucial for reconstructing damaged liver cells. However, use caution. Cirrhosis may make it difficult for the liver to process large quantities of protein efficiently.
Consuming too much protein can lead to hepatic encephalopathy. This is because the liver manufactures ammonia when it metabolizes protein.
As mentioned earlier, cirrhosis may impair the liver’s ability to get rid of ammonia from the body. If that happens, the excess ammonia builds in the blood stream and eventually makes its way to the brain, with the resultant confusion and fatigue.
Everyone is different, so experiment with your protein intake. Not too much but not too little.
Don’t neglect coffee. Studies have shown that coffee can protect the liver, especially in those with NAFLD.
Healthy fats such as avocados, olive oil, walnuts, and almonds are beneficial. Keep a limit on saturated fats, and keep trans fats off-limits.
Fish, garlic, onions, and white meat should also be a part of your liver-friendly diet. Also, consume a significant amount of complex carbohydrates (oatmeal, brown rice, peas, lentils, quinoa, and beans) and keep simple carbs like white rice, white bread, and baked goods to a minimum, or eliminate them altogether.
Finally, avoid high-fructose corn syrup (HFCS) like the plague. When you eat or drink HFCS, it speeds directly to your liver. This is a problem with people with cirrhosis. With that condition the liver is working overtime; why add to its overload by making it work even harder?
Sodas and sweetened drinks are the main offenders when it comes to HFCS. But this hazardous substance can sneak its way into your system in food. The takeaway? Read labels!
Start a Liver Detoxification Plan
Stay hydrated. Drink healthy, pure filtered water daily. Upon awakening, fresh-squeezed lemon water will get your liver going on the right track.
The good idea is to divide your weight in half, then consume that amount of water in ounces daily. Forget about that stuff that flows from your tap. Install a reverse osmosis water filter to ensure your water does not contain any toxic substances or traces of prescription drugs.
Alkaline water and mineral water are also excellent choices.
 Stop drinking alcohol. For some, this is challenging, to put it mildly. But alcohol is hard to handle for a healthy liver. If you are suffering from cirrhosis, stopping drinking is not optional.
Stop drinking alcohol. For some, this is challenging, to put it mildly. But alcohol is hard to handle for a healthy liver. If you are suffering from cirrhosis, stopping drinking is not optional.
Alcohol will continue to destroy what’s left of your liver and undermine the positive things you are doing to help your liver recover.
Avoid sugar, artificial sweeteners, alcohol, soda, processed or preserved foods, fast foods, simple carbohydrates, and white flour products.
Consider juicing. Juicers are reasonably priced and are an excellent way to feed your body the extra nutrition it needs to ease your liver’s burden. When choosing fruits, look for those on the lower end of the glycemic index (apples, blueberries).
Broccoli, carrots, spinach, celery, and kale are good choices for adding vegetables to the mix.
Done correctly, juicing is a powerful, anti-oxidant punch.
Maintain a healthy lymphatic system. Think of your lymphatic system as the body’s "sewer system.” The body contains twice as much lymph fluid as blood, and twice the number of lymph vessels compared to blood vessels.
Since the lymph system has no pump, it relies on breathing to make a partial vacuum that forces blood and lymph to flow upward, then reverses and flows back down to the bloodstream.
Therefore, deep breathing is critical. For starters, engage in deep breathing for a few minutes twice daily. Also, consider the practice of Chi Kung, an ancient healing system based on a variety of deep breathing and flowing gentle exercises.
A practice of meditation can also help control stress. Added pressure is not something you need when battling cirrhosis.
Beware of certain medicines, both over-the-counter and prescriptions. Acetaminophen (Tylenol) is safe to take as recommended. However, be aware that it is a primary cause of liver failure when taking massive doses over a brief time. Acetaminophen is also in Percocet and Vicodin.
Antibiotics, Non-steroidal Anti-inflammatory Drugs (NSAIDs), and statins can also wreak havoc with your liver.
As always, check with your doctor before taking any of these substances.
Supplements that May Hurt and Supplements that May Help
The use of nutritional supplements can be both good and bad. Here is a list of supplements that may damage your liver:
Kava Kava.
Comfrey.
Chaparral.
Yohimbine.
Skullcap.
Certain weight-loss pills or powders.
Excess iron.
Excess vitamin A.
The rule with these supplements is elementary. They may not harm everyone who uses them in moderation. But before taking any of them, check with your doctor.
Here is a list of liver-supporting supplements:
Milk thistle
N-acetylcysteine
Alpha-lipoic-acid
Vitamin B
Probiotics
Selenium
Phosphatidylcholine (PC)
Melatonin
Tumeric
None of these supplements are miracle workers. By themselves, they WILL NOT cure cirrhosis. But they can be useful additions to your liver-friendly toolbox.
At the risk of redundancy, always check with your physician before taking any nutritional supplement.
The Importance of Exercise
The broad range of benefits exercise delivers is well-known: lower blood pressure, blood sugar regulation, better circulation, boosts heart health and lowers cholesterol levels.
cholesterol levels.
The best news? Physical fitness also helps the liver.
The catch is this. Cirrhosis can cause fatigue and lethargy. Often those with cirrhosis just don’t feel like exercising.
However, a good workout can skyrocket your metabolism and give your energy levels a much-needed boost.
The first step in any fitness activity is to get clearance from your doctor. As mentioned earlier, liver disease can spill over into other organs and cause multiple problems.
So discuss your fitness plans with your doctor. Start small. There’s no need to spend hours in the gym or start preparing to run a marathon.
Your goal is to develop a well-balanced exercise routine. Aerobic training for endurance, resistance training for strength, and stretching for flexibility are a good foundation.
Stem Cells – a Possible Cirrhosis Cure?
Currently, there is no cure for cirrhosis. Its advance can be slowed and perhaps halted. But there is currently no way to regenerate the dead liver cells that have hardened.
However, research is continuing on several fronts. And that includes research into ways to use induced pluripotent stem cells (iPSCs) to regenerate diseased  livers and prevent liver failure.
livers and prevent liver failure.
Unlike the controversy created concerning embryonic stem cells harvested from human embryos, iPSCs are made from adult stem cells and can be generated from the patient's body.
Using stem cells derived from the patients own bodies to make new liver tissue that will be placed back into their livers could eliminate the need for organ donors (for which there is a critical shortage of liver donors).
In spite of the tremendous potential iPSCs hold for regenerative medicine, the technology is not there yet and could be a decade away before iPSCs can be deployed safely and efficiently.
Therefore, if you are currently dealing with cirrhosis, it is important not to give up hope. Follow the ideas in this article. Stay as healthy as possible, and take comfort that cirrhosis cures are on the way.
References
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- Are You Constantly Feeling Tired And Fatigued ? [Last Updated On: May 21st, 2024] [Originally Added On: May 1st, 2018]
- Constantly Tired? Can't Sleep? [Last Updated On: April 10th, 2024] [Originally Added On: March 23rd, 2019]
- Insomnia: The Silent Killer [Last Updated On: April 8th, 2024] [Originally Added On: April 30th, 2019]
- Lipocine Reintroduces Tlando [Last Updated On: July 18th, 2024] [Originally Added On: March 18th, 2020]
- High-Intensity Interval Training Boosts Both Body and Mind [Last Updated On: February 20th, 2025] [Originally Added On: May 10th, 2020]
- Tattoo Safety: What to Know Before You Get a Tattoo [Last Updated On: April 1st, 2024] [Originally Added On: June 2nd, 2020]
- Testosterone and Fatherhood [Last Updated On: May 20th, 2024] [Originally Added On: October 12th, 2020]
- L-Arginine: The Key to Both Heart Health and Sexual Health [Last Updated On: April 6th, 2024] [Originally Added On: December 4th, 2020]
- The Importance of Hormonal Balance for Menopause [Last Updated On: February 20th, 2025] [Originally Added On: December 14th, 2020]
- Menopause Drugs: Study Stokes New Debate Over Cancer Risks [Last Updated On: April 4th, 2024] [Originally Added On: December 16th, 2020]
- Study Examines Link Between Growth Hormones and Osteoporosis [Last Updated On: April 7th, 2024] [Originally Added On: December 17th, 2020]
- Everything You Need to Know About Clomiphene [Last Updated On: April 5th, 2024] [Originally Added On: December 20th, 2020]
- Fast Facts About DHEA: What You Need to Know About This Natural Steroid [Last Updated On: July 15th, 2024] [Originally Added On: March 4th, 2021]
- Enjoy a Few Drinks Weekly? Beware: This May Be a Link to Low Sperm Counts and Quality [Last Updated On: April 2nd, 2024] [Originally Added On: August 16th, 2021]
- Hormone Therapy May Benefit Some Women's Hearts [Last Updated On: February 20th, 2025] [Originally Added On: August 18th, 2021]
- HGH Male Blood Panel [Last Updated On: October 28th, 2021] [Originally Added On: September 28th, 2021]
- Growth Hormone Battles Osteoporosis [Last Updated On: March 31st, 2024] [Originally Added On: October 11th, 2021]
- Growth hormone = More Sleep = Better Sex! [Last Updated On: April 3rd, 2024] [Originally Added On: October 11th, 2021]
- Low Testosterone and Hypogonadism: The Difference [Last Updated On: June 10th, 2024] [Originally Added On: October 12th, 2021]
- The Link Between Testosterone and Tylenol [Last Updated On: March 26th, 2024] [Originally Added On: October 12th, 2021]
- Hormone Replacement Therapy and Aerobics May Ease Menopause Symptoms [Last Updated On: February 19th, 2025] [Originally Added On: October 13th, 2021]
- Growth Hormone and Lifestyle = An Extended Lifespan [Last Updated On: March 28th, 2024] [Originally Added On: October 13th, 2021]
- Growth Hormone, Foods, and Supplements for Healthy Skin [Last Updated On: June 1st, 2024] [Originally Added On: October 13th, 2021]
- Hormone Replacement Therapy, Menopause, and Cancer [Last Updated On: March 29th, 2024] [Originally Added On: October 13th, 2021]
- Growth Hormone, Exercise, and Osteoporosis: The Facts! [Last Updated On: March 27th, 2024] [Originally Added On: October 13th, 2021]
- Hormone Replacement Therapy and Menopause [Last Updated On: March 30th, 2024] [Originally Added On: October 13th, 2021]
- Testosterone and Women [Last Updated On: February 18th, 2025] [Originally Added On: October 13th, 2021]
- Growth Hormone and Smoking [Last Updated On: February 19th, 2025] [Originally Added On: October 14th, 2021]
- Testosterone, Statins, and Prostate Cancer [Last Updated On: February 18th, 2025] [Originally Added On: October 19th, 2021]
- Researchers Investigate Declining Sperm Counts, Find Chemicals Rampant [Last Updated On: June 14th, 2024] [Originally Added On: June 14th, 2022]
- Understanding the Role of Hormonal Balance in Menopause [Last Updated On: February 7th, 2025] [Originally Added On: February 7th, 2025]
- Introduction: Benefits of Hormone Replacement Therapy [Last Updated On: February 8th, 2025] [Originally Added On: February 8th, 2025]
- The Influences and Benefits of High-Intensity Interval Training [Last Updated On: February 8th, 2025] [Originally Added On: February 8th, 2025]