Video Link: https://vimeo.com/288017209
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Video Link: https://vimeo.com/288017913
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Did you know:
Low Testosterone levels can predict Metabolic Syndrome
Testosterone protects against Multiple Sclerosis
Testosterone may protect men from autoimmune disease
Testosterone Therapy may reduce men’s risk of Prostate Cancer
Keep reading and discover the many exciting and little-known benefits of this miraculous hormone
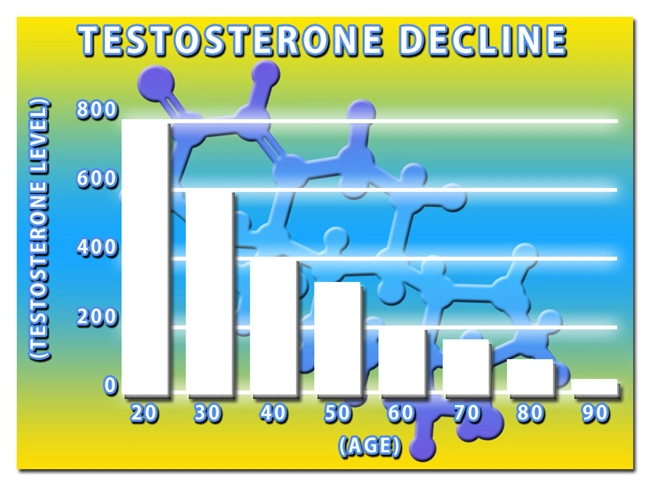
Testosterone. The male hormone responsible for muscles, manhood, and chest hair. This potent hormone is also behind the male sex drive, risk-taking, courage, aggression, and a broad range of definitive masculine characteristics, both good and bad, depending on circumstances.
But Testosterone Also Plays a Critical Role in Maintaining Men’s Health
That’s correct. A recent study confirmed that total testosterone (TT) and sex-hormone-binding globulin (SHBG) add pieces to the puzzle of predicting the development of the dreaded metabolic syndrome (MetS)
 The metabolic syndrome manifests in several different ways, and none of them are welcome: increased blood sugar levels, weight gain, elevated cholesterol and triglyceride levels, high blood pressure – all of which dangerously increase the risk of severe adverse health conditions: diabetes, stroke, cancer, and heart attack. A line-up that no one wants or needs.
The metabolic syndrome manifests in several different ways, and none of them are welcome: increased blood sugar levels, weight gain, elevated cholesterol and triglyceride levels, high blood pressure – all of which dangerously increase the risk of severe adverse health conditions: diabetes, stroke, cancer, and heart attack. A line-up that no one wants or needs.
The one-year study began in October 2016 in Faiha Specialized Diabetes, Endocrine, and Metabolism Center (FDEMC) in Basrah, Iran, and included 169 obese people (89 women and 80 men).
The study concluded that both TT and SHBG were substantially lower in obese men with MetS compared with non-obese men. In obese women, there was no significant disparity in SHBG with non-obese women.
Before we go any further, a definition of both total testosterone and sex-hormone-binding globulin is in order.
The Crucial Difference Between Free Testosterone (FT) and Bound Testosterone
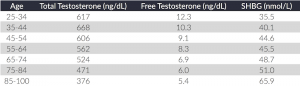
There is a common misconception that a testosterone blood test should only measure total testosterone. But this doesn’t tell the entire story…by a long shot!
In healthy men, only a small percentage (1-3%) of total testosterone is free testosterone (“FT”). Free testosterone is the testosterone that travels through the blood stream, enters the muscles and cells, and performs its vital functions of keeping men robust and reducing fat cells.
The vast majority of testosterone is shackled to sex hormone-binding globulin. As men age, this ratio gets worse – less FT is accessible, and more testosterone is bound to SHBG.
The result? Less free testosterone, which creates a perfect environment for a series of enfeebling side effects: muscle weakness, diminished libido, cognitive impairment, joint aches and pains, stiffness, depression, and an all-around drop in a man’s quality of life.
The key takeaway is this: if you feel you may be suffering from Low-T, and are considering getting a blood test to confirm your suspicions, make sure that you don’t solely rely on your total testosterone level.
The ratio of FT to SHBG is more significant than total testosterone. This ratio illustrates the importance of keeping SHBG levels in check.
Therefore, make sure your testosterone blood test includes both measurements and pay attention to that all-important ratio.
More Good Testosterone News
The rumors and fear-mongering concerning testosterone replacement therapy (TRT) continue, at times unabated. This cacophony is especially deafening  concerning the so-called “link” between testosterone and prostate cancer (PCa).
concerning the so-called “link” between testosterone and prostate cancer (PCa).
Logically, this link makes no sense. Prostate cancer is mostly a disease affecting older men. The Prostate Cancer Foundation reports that the older a man is, the more likely he will be diagnosed with the disease. The odds of receiving a prostate cancer diagnosis are a mere 1 in 403 for men under the age of fifty.
However, those odds dramatically increase with age. The rate explodes to 1 in 58 for men ages 50-59 and 1 in 21 for ages 60-69.
Based on these numbers it is safe to arrive at the following conclusion.
Since young men who are full of testosterone seldom get prostate cancer while older men with diminished levels of the hormone are far more likely to be stricken with the disease, perhaps testosterone is not the primary culprit in the development of prostate cancer.
A Recent Study Confirmed This Theory
Physicians Ahmad Haider, MD, and Karim Sultan Haider, MD, who practice medicine in Bremerhaven, Germany, studied 762 men with testosterone levels of 350 ng/dl or lower. Of this total, 412 men received testosterone undecanoate -- 1,000 mg every three months for as long as 12 years. The remaining study participants (the control group) did not receive any testosterone replacement therapy.
The average follow-up time was nine years. And the total participant time was approximately 6,400 patient years.
The results of the study were surprising. Eleven men who received testosterone replacement therapy (2.7%) were diagnosed with prostate cancer. In the control group that did not receive TRT, 34 men (8.9%) were diagnosed with the condition.
 Also, the mean age of the men in the TRT group was 65.2 compared to 54.3 in the control group.
Also, the mean age of the men in the TRT group was 65.2 compared to 54.3 in the control group.
Finally, the study determined that the cancer was less rigorous in the TRT group.
“In the testosterone group, all prostate cancers were diagnosed within the first year and a half suggesting that cancers had been present before initiating testosterone therapy,” Dr. Haider said. “Because low testosterone is associated with low PSA, hypogonadism may contribute to the reduced detectability of prostate cancer. Normalizing testosterone may have brought out occult cancer.”
He added: “Our registry is ongoing, and we keep following our patients year after year. The results are getting more robust with advancing time.”
A Veterans Administration Study has Similar Conclusions
In another study, 147,593 US veterans suffering from low testosterone were monitored for approximately three years. This was a controlled study with 56,833 participants (40%) receiving TRT. Of this group, 38% were treated solely with topical testosterone, 40% received intramuscular testosterone only, and the remaining 22% were administered both types of testosterone treatments.
The lead physician for the study was Dr. Thomas J. Walsh, MD, from the University of Washington in Seattle. Dr. Walsh and his fellow researchers found that prostate cancer occurrence was 2.27 per 1,000 person-years for men receiving TRT, while the rate of prostate cancer was 2.60 in the same time frame for men in the control group receiving no testosterone.
The conclusion was obvious. There was no link between testosterone replacement therapy and increased risk of prostate cancer. This was true regardless of the length and amount of TRT.
“Among veterans with low testosterone levels, compared to no treatment, testosterone treatment was not associated with increased risk of subsequent prostate cancer diagnosis, and prostate cancer, or high grade” Dr. Walsh proclaimed in a press conference.
More Evidence of Testosterone’s Protection
Still another study concerning testosterone (“T”) and prostate cancer risk was conducted by lead researcher Xiaohui Xu, Ph.D., of Texas A&M University in College Station, Texas, and his research team.
The researchers monitored 376 men with low testosterone who did not undergo TRT. The age range of the participants was 45 to 74 years, and they were tracked for between 2 through 11 years. During that time, 26 men developed prostate cancer.
Here’s the significance of that study. The risk for prostate cancer DROPPED for the men who kept their testosterone levels above 12.1 nmol/L. The researchers determined that men who suffered massive drops in testosterone were more apt to develop prostate cancer. This was especially true if these testosterone losses occurred at younger ages.
 In other words, the longer the testosterone level remains above the 12.1 nmol/L, the lower the risk of prostate cancer. The cancer risk plunged by 32% for every 1-year increase in age when diagnosed.
In other words, the longer the testosterone level remains above the 12.1 nmol/L, the lower the risk of prostate cancer. The cancer risk plunged by 32% for every 1-year increase in age when diagnosed.
The more a man’s testosterone fluctuated over time, the risk of prostate cancer increased nearly five-fold!
Worse, if a man suffered an enormous drop in testosterone that exceeded 20% of his average, or a relatively substantial median slide within two years increased their cancer risk by 8.5 and 2.7 respectively.
The family history of PCa, alcohol use, body mass index (BMI), and smoking were all factors considered.
“Our study is the first to provide evidence of the association between dynamic patterns of T and PCa development and may have substantial clinical impacts on PCa prevention,” Xu wrote.
The researchers hypothesized that healthy prostate cells have a reasonable range of testosterone that differs from individual men. Unusual testosterone drops in an individual possibly distort the firm, fixed environment inside the prostate and result in cellular changes that may set the stage for prostate cancer.
“Maintaining T levels stable may have a significant impact on PCa prevention” Dr. Xu and his team concluded. He added that “Also, regular monitoring of T levels in males may be useful earlier in life, e.g., at 40-50 years of age, to establish a baseline from which changes could then be detected.”
The parade of testosterone’s benefits keeps coming. Here’s more...
Testosterone May Protect Men From Autoimmune Diseases
A curious statistic: women are three to nine times more apt than men to be hit with a broad range of autoimmune diseases: systemic lupus erythematosus, celiac disease, Graves disease, multiple sclerosis (MS), and rheumatoid arthritis.
 In addition to suffering from these conditions more often than men, women also get them at earlier ages than men.
In addition to suffering from these conditions more often than men, women also get them at earlier ages than men.
Why is this? One theory explains the difference in the occurrence of these diseases between men and women as a direct result of testosterone.
Men have far more testosterone circulating in their blood than women; as much as eight times more.
Tests on mice have concluded that testosterone protects from MS. The focus of the trial was on mast cells.
What is a Mast Cell?
The dictionary definition of a mast cell is a cell filled with basophil granules, found in numbers in connective tissue and releasing histamine and other substances during inflammatory and allergic reactions.
The crucial word in that definition was inflammatory. In a recent study on MS using mice, testosterone altered the action of mast cells in the central nervous system, the lymph nodes, and the lining of the brain.
In female mice mast cells pumped out signaling molecules called Th17 Cytokines, which cause inflammation. This type of cytokine attacks myelin.
Myelin acts as a sheath that surrounds the axon of some nerve cells and forms an electrically insulating layer of protection. When myelin is destroyed, nerve signals and communication slows down and may even stop.
This loss of myelin protection is the primary cause of autoimmune disorders, especially MS. Weakened myelin is a significant factor in the progression of the  disease.
disease.
Female mice, like human females, produce fewer amounts of testosterone than males.
Here’s the fundamental fact: when mast cells located in those crucial areas mentioned earlier are treated with testosterone, a dramatic change happens. Instead of producing Th17 cytokines that cause inflammation, testosterone causes the cytokines to lower inflammation.
This action is a result of testosterone causing mast cells to produce cytokine IL-33 in male mice, which opens a floodgate of chemicals to stop Th17 immune cells from attacking the myelin.
The study observed male mice with low testosterone levels that had few or no interleukin-33 (IL-33) mast cells and noted that MS acted similarly to the manner it advances in female mice.
The researchers concluded that testosterone was the critical element in stopping the advancement of MS.
The results of the study were published in the Proceeding of the National Academy of Sciences.
“This suggests a mechanism for the reduced incidence of multiple sclerosis and other autoimmune diseases in males compared to females” according to lead study author Melissa Brown, Ph.D. She added that “These findings could lead to an entirely new kind of therapy for MS, which we greatly need.”
“Because testosterone levels were seven to eight times lower in adult women compared to men, we speculate there are insufficient levels in females to activate this protective pathway,” Dr. Brown stated.
“But we showed we could activate the pathway with the guardian molecule IL-33.”
The hope is that women can also enjoy testosterone protection. “This is why it’s vital to study sex differences in research,” Dr. Brown added.
The study also noted that men who developed multiple sclerosis later in life are linked to lower testosterone levels.
The good news? Several clinical trials that included men with MS have shown that testosterone replacement therapy can somewhat reverse myelin damage and ease the debilitating symptoms of MS.
Also, there is hope for successfully treating women with testosterone, as well as men.
Dr. Brown concluded that “Our findings have identified new and more specific cellular and molecular targets for immune intervention that we hope will lead to better therapies that leave most of the immune system intact. This testosterone-driven protective pathway should also be studied in other female-biased autoimmune diseases.”
The two drugs that presently are approved for MS treatment work by altering the T cells in MS patients to resemble the T cells in male mice, which lower  inflammation rather than elevate it.
inflammation rather than elevate it.
Research into curing the terrible disease of multiple sclerosis may result in the cytokine IL-33, which is the cytokine testosterone causes mast cells to produce, being added to the tools to eradicate MS once and for all.
No question about it. Medical research continues to discover the numerous benefits of testosterone. And the investigation is advancing at a blistering pace. Our clinic has the tools, the experience, and the know-how to deliver these cutting-edge benefits to you.
References
A comprehensive review on metabolic syndrome.
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- LabCorp Announces a Change to the Testosterone Reference Range [Last Updated On: May 11th, 2024] [Originally Added On: June 23rd, 2019]
- Important Facts About Testosterone Therapy Before Buying [Last Updated On: May 13th, 2024] [Originally Added On: July 13th, 2019]
- Soy: Does it Lower Testosterone? [Last Updated On: October 18th, 2024] [Originally Added On: August 30th, 2020]
- Testosterone Treatments May Successfully Reverse Type-2 Diabetes in Some Men [Last Updated On: April 15th, 2025] [Originally Added On: November 13th, 2020]
- Testosterone Replacement Therapy (TRT) May Prevent Heart Attacks and Diabetes [Last Updated On: May 16th, 2024] [Originally Added On: November 17th, 2020]
- Did You Know? Recent Studies Have Confirmed the Link Between Low Testosterone (“Low-T”) and Depression. [Last Updated On: May 12th, 2024] [Originally Added On: January 10th, 2021]
- New Study Finds Testosterone Does Not Increase Your Heart Attack Risk [Last Updated On: April 14th, 2025] [Originally Added On: January 11th, 2021]
- The Great Testosterone Debate [Last Updated On: May 15th, 2024] [Originally Added On: January 14th, 2021]
- Testosterone Replacement Therapy Lowers Heart Attack Risk [Last Updated On: May 14th, 2024] [Originally Added On: January 18th, 2021]
- New Study Says: The Benefits of Testosterone Replacement Therapy Outweigh The Risks [Last Updated On: May 17th, 2024] [Originally Added On: January 19th, 2021]
- Male Menopause. Fact or Fiction ? [Last Updated On: May 18th, 2024] [Originally Added On: January 20th, 2021]
- Testosterone: How Much Do You Really Know About This Masculine Hormone? [Last Updated On: October 6th, 2024] [Originally Added On: February 9th, 2021]
- Low-T: What are healthy levels of Testosterone and why is it difficult to measure? [Last Updated On: August 10th, 2024] [Originally Added On: April 3rd, 2021]
- Testosterone Therapy May Be Good for the Heart if You Have Low-T [Last Updated On: May 27th, 2024] [Originally Added On: July 21st, 2021]
- A Recent Study Concludes: Testosterone DOES NOT Cause Prostate Cancer [Last Updated On: August 14th, 2024] [Originally Added On: August 16th, 2021]
- In the Battle Against Aging, When do the Risks Outweigh the Rewards? [Last Updated On: April 4th, 2025] [Originally Added On: August 18th, 2021]
- New Study Concludes: Boosting Testosterone Levels Lowers Men's Death Risk [Last Updated On: June 2nd, 2024] [Originally Added On: August 20th, 2021]
- Testosterone Replacement Therapy Slows Prostate Cancer! [Last Updated On: April 2nd, 2025] [Originally Added On: September 13th, 2021]
- Research proves that Testosterone Therapy Boosts Fertility! [Last Updated On: April 5th, 2025] [Originally Added On: September 26th, 2021]
- Free Testosterone and Sex Hormone-Binding Globulin [Last Updated On: April 6th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone Does Not Cause Heart Attacks [Last Updated On: April 7th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Women [Last Updated On: April 8th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Disease Prevention [Last Updated On: March 31st, 2025] [Originally Added On: October 15th, 2021]
- Judge Vacates $140 Million Verdict in Testosterone Lawsuit [Last Updated On: April 1st, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Estrogen [Last Updated On: April 9th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone and Aging [Last Updated On: April 10th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone Replacement Therapy (TRT) Benefits [Last Updated On: April 11th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone and Male Menopause [Last Updated On: March 30th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone Battles Obesity [Last Updated On: March 29th, 2025] [Originally Added On: October 16th, 2021]
- Why You Need Testosterone Replacement Therapy [Last Updated On: June 5th, 2024] [Originally Added On: October 16th, 2021]
- Testosterone FAQ's [Last Updated On: June 4th, 2024] [Originally Added On: October 25th, 2021]
- How Testosterone Impacts Sexual Preferences In Men and Women [Last Updated On: March 28th, 2025] [Originally Added On: October 30th, 2021]
- Growth Hormone and The Thyroid Gland [Last Updated On: May 19th, 2024] [Originally Added On: November 19th, 2021]
- How Does Masturbation Affect Testosterone Levels? Exploring the Science [Last Updated On: June 15th, 2024] [Originally Added On: March 27th, 2022]
- Testosterone Therapy Increasingly Used to Help Men Take Control of Aging [Last Updated On: June 16th, 2024] [Originally Added On: May 30th, 2022]
- The many benefits of Testosterone Replacement Therapy (TRT) [Last Updated On: October 1st, 2024] [Originally Added On: June 13th, 2022]
- Tlando Testosterone - A Brand New Way to Treat Low-T Safely with a Testosterone Pill [Last Updated On: June 19th, 2024] [Originally Added On: July 12th, 2022]
- Safe Tlando Testosterone Changes Landscape of Low-T Therapy [Last Updated On: June 21st, 2024] [Originally Added On: August 15th, 2022]
- Systems to Monitor Testosterone Replacement Therapy (TRT) [Last Updated On: September 11th, 2024] [Originally Added On: September 21st, 2022]
- Testosterone May Help You Keep Your Job (Or Find Another) [Last Updated On: July 4th, 2024] [Originally Added On: October 4th, 2022]
- Toxic Chemicals are Killing your testosterone…And your Manhood! [Last Updated On: October 28th, 2024] [Originally Added On: October 10th, 2022]
- A new study reveals that Testosterone improves body composition in men with low testosterone! [Last Updated On: September 21st, 2024] [Originally Added On: October 17th, 2022]
- A former Mr. Olympia speaks about testosterone [Last Updated On: September 9th, 2024] [Originally Added On: November 8th, 2022]
- Testosterone Blockers Thwart Melanoma [Last Updated On: July 1st, 2024] [Originally Added On: December 11th, 2022]