Video Link: https://vimeo.com/282203004
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Video Link: https://vimeo.com/282202848
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
With the constant drumbeat of headlines in the news about the risks of Testosterone, it would be easy to believe that there are no health benefits in  Testosterone Replacement Therapy (TRT) for middle-aged men, only health hazards.
Testosterone Replacement Therapy (TRT) for middle-aged men, only health hazards.
Heart attacks and strokes are mentioned prominently in the television advertisements by law firms that are just lying in wait to file lawsuits against the Testosterone manufacturers.
If that weren't bad enough, there is a seemingly endless trail of “recommendations” by “medical experts,” including the Food and Drug Administration (FDA), that call for severe restrictions on a physician's ability to prescribe Testosterone for general health and anti-aging.
However, there are two sides to every story, and for the most part, we only hear one side: the negative.
But more and more studies are discovering that low Testosterone (“low-T”) may be a far more significant problem than any complication from Testosterone Replacement Therapy.
For example, a recent Houston-area study concluded that Testosterone replacement for men with little or no amounts of this hormone did not increase the risk of a heart attack.
The study, conducted by researchers at the University of Texas Medical Branch at Galveston, refutes the notion that Testosterone therapy increases a man's risk of a heart attack.
Testosterone is a very timely topic since more men than ever are supplementing Testosterone to prevent or delay the maladies of aging.
"Testosterone's perceived risk and impact on patients have been in the news a lot lately," said Jacques Baillargeon, a UTMB professor of epidemiology and the  study's lead author.
study's lead author.
"I hope this study brings some balance to the debate, that it's weighed alongside all the evidence."
Baillargeon, whose 2013 research documented a tripling in Testosterone use in the past decade, said he conducted the new study because of confusion about Testosterone's effect.
Before recent studies found a cardiovascular risk, he noted a significant body of evidence that exposed the treatment does not increase the possibility of a heart attack.
Baillargeon admitted that the retrospective study isn't likely to be "the final word on the subject" and said a large-scale, randomized trial is needed to provide more definitive evidence.
The Food and Drug Administration approved testosterone therapy in the 1950s for men whose doctors diagnosed hypogonadism, which occurs when the function of the testicles is impaired.
Some men are born with hypogonadism, while others develop it later in life, typically due to injury or illness.
But thanks to several advertising campaigns touting pills, patches, and formulations for men with "Low-T," Testosterone is now a $1.6 billion market.
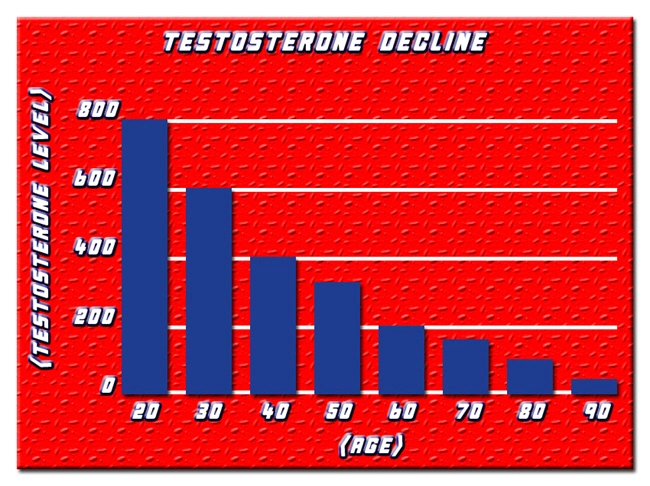
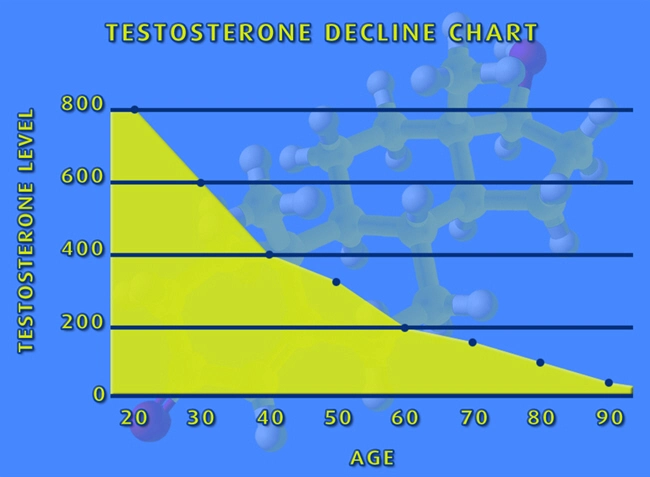
The ads claim the products boost libido, energy, and muscle tone, which they state decrease because Testosterone levels decline roughly 1 per cent a year after age 35.
But as with all things concerning health, there's considerable debate in the medical community, which questions whether the therapy provides such benefit.
The FDA is still weighing the evidence, but an advisory panel recommended the agency restrict Testosterone therapy to recently diagnosed cases of hypogonadism, meaning companies couldn't market it for age-related Testosterone decline.
The FDA is not required to follow the recommendations of its advisory panels but usually does.
The group delved into safety risks, including the recent studies, and concluded that the evidence for risks of cardiovascular problems was uncertain.
All but one  of the members voted to require clinical trials for safety for at least some types of Testosterone therapy.
of the members voted to require clinical trials for safety for at least some types of Testosterone therapy.
Baillargeon's study was published in the Annals of Pharmacology.
It not only concluded that Testosterone therapy prescribed for diagnosed cases of hypergonadism was not associated with an increased risk of a heart attack.
It also discovered that such patients with a higher probability of cardiovascular problems had a lower rate of heart attacks compared to patients with the same likelihood of cardiovascular issues who received no Testosterone therapy.
Testosterone cut the risk by 30 percent!
"Based on recent studies, there has been concern about treating hypogonadism with testosterone, but based on our study, there should also be concern about not treating the condition with testosterone," Baillargeon said.
Baillargeon added that the finding that Testosterone is protective needs to be replicated in future studies.
He said the FDA panel's recommendation "sounds reasonable while we await the results of the major clinical trials."
For those with normal or low-normal Testosterone, as opposed to hypogonadism, he said, the risk-benefit ratio seems unfavorable.
Baillargeon's team compared Medicare records of 6,355 men who had at least one injection between 1997 and 2005 with 19,065 non-Testosterone users.
Patients receiving the therapy had an average of 8.2 injections over the study period, including 4.4 in the first year. They were more likely to have a high degree of co-morbid disease than non-users.
Gel, patch, and oral formulations are now more commonly used than they were during the study period, but, Baillargeon said, if anything, injections would be  expected to be higher.
expected to be higher.
The research was funded by the National Institutes of Health and the Agency for Healthcare Research and Quality.
And Another Study Agrees...
In another study, research again concludes that Low-T may signify that men face an elevated risk of sudden cardiac arrest.
An investigation team from Cedars-Sinai Heart Institute, which published its findings in Heart Rhythm, evaluated Testosterone levels in 149 patients who suffered unexpected attacks and found uncommon cases of Low-T with the men and unusually soaring estradiol levels in both the men and the women.
“Because [sudden cardiac arrest] is usually fatal, we are constantly looking for ways to predict which patients are susceptible so we can concentrate on prevention,” said study author Sumeet Chugh, MD, in a news release that accompanied the publication of the results.
“If we wait until someone has a sudden cardiac arrest, it is usually too late for treatment.”
Chugh and his team compared hormone levels from the subjects who experienced a heart attack with those from a group of similar control subjects.
The median Testosterone level for men who experienced cardiac arrest was 4.4 ng/mL.
The median Testosterone level for men from the control group was 5.4 ng/mL (P =.01).
Testosterone levels did not differ significantly between women in the study and control groups.
Median estradiol levels, however, varied between victims and controls for both men (68 pg/mL vs. 52 pg/mL; P<.001) and women (54 pg/mL vs. 36 pg/mL; P<.001).
Multivariate analysis indicated higher Testosterone levels were linked with a substantially lower risk of sudden cardiac arrest for men (odds ratio [OR] = 0.75; 95% CI, 0.58-0.96).
The association between high estradiol levels and the increased risk was even more profound in both men (OR=2; 95% CI, 1.5-2.6) and women (OR=3.5; 95% CI, 1.9-6.4).
High testosterone to estrogen ratios was related to considerably reduced risk in men (OR=0.5; 95% CI, 0.4-0.7) but not in women.
“This is the first time it has been reported that there is an association between sex hormone levels and [sudden cardiac arrest],” Chugh said. “While these findings need to be confirmed by other studies, they suggest that higher testosterone levels in men may offer protection from sudden cardiac arrest and lower levels of estrogen may protect both men and women.”
The recent research delivers additional evidence that rather than hurt the heart, Testosterone actually provides cardiovascular protection. But the issue is far from settled as other studies have arrived at different conclusions.
Since the publication of two detailed studies that connected testosterone therapy with adverse events, the FDA has been looking into the matter.
The first study, published in JAMA, uncovered a strong, positive connection between Testosterone therapy and the increased possibility of stroke, myocardial infarction (MI), and death.
The second study, published in PLoS ONE, linked testosterone therapy with a significantly higher risk of heart disease for older and younger men with a history of heart disease.
However, the PloS study was loaded with flaws.
Here is the main one: the authors of the survey compared the groups of men started on Testosterone therapy to men started on PDE5 inhibitors and found a lower risk of heart disease in the PDE5 inhibitor group.
PDE5 inhibitors are drugs used to treat men  with erectile dysfunction (Viagra and others are in this class). The authors state they used this group, so there would theoretically be an increase in sexual activity in both teams.
with erectile dysfunction (Viagra and others are in this class). The authors state they used this group, so there would theoretically be an increase in sexual activity in both teams.
They ignored one vital point, though.
PDE5 inhibitors work throughout the body and have substantial positive effects on the cardiovascular system.
Two of the PDE5 inhibitors were approved for the treatment of idiopathic pulmonary hypertension because of the ability of PDE5 inhibitors to relax blood vessels.
This month, a new study in the Journal of Cardiovascular Pharmacology and Therapeutics states that PDE5 inhibitors have potential as cardiovascular drugs in patients with coronary artery disease and even possible improvement in heart failure patients.
With the data that PDE5 inhibitors can decrease the risk of heart disease and help to relax blood vessels in men with cardiovascular disease, the authors never should have concluded that men on PDE5 inhibitors would be a good control group against the men placed on Testosterone therapy.
However, since that time, journals have published studies that have connected testosterone therapy (or higher Testosterone levels) with cardiac health.
The most significant of those, an analysis of records from 25,000 patients, detected no link between Testosterone therapy and MI but a strong negative relationship between treatment and MI among the 25% of men who faced the highest risk of MI.
The result?
The confusion over this issue rages on.
Recently, in another study, the FDA said there’s no compelling evidence of any sizeable link between testosterone therapy and adverse cardiovascular events.
Two FDA advisory committees will confer at a later date to consider the matter further.
The Most Recent FDA Recommendations
As mentioned earlier, another FDA committee voted 20 to 1 to make it more difficult for doctors to prescribe Testosterone products.
The committee also recommended that pharmaceutical companies that sell Testosterone products be required to perform additional safety tests, based mostly on a few studies indicating that patients with heart problems are more likely to experience cardiac events when they start using Testosterone.
This is a case of deja vu.
 At one time, it was believed that Testosterone significantly increased the risk of prostate cancer.
At one time, it was believed that Testosterone significantly increased the risk of prostate cancer.
The prostate cancer link has been widely discredited, and the hormone is now prescribed widely.
As aging baby boomers flood into the realm of andropause, the use of Testosterone Replacement Therapy has exploded.
Men who use the products often experience increased muscle mass, bone density, libido, deeper sleep, and a sense of well-being.
If true, this raises even more questions, because the inability to sleep is linked to all manner of conditions including Alzheimer’s, diabetes, and heart disease.
Many people report an improvement in their Body Mass Index (BMI).
A presentation given at the American Urological Association Annual Scientific Meeting in 2012 reviewed two studies that demonstrated dramatic improvements in body weight for subjects taking testosterone undecanoate, a long-acting form of the hormone available in Germany.
The weight loss reported in studies could significantly improve health for overweight men.
On the other side of the scale, some people with preexisting heart conditions might experience an increase in cardiac problems during the first few months of usage.
The science, however, remains unsettled.
Some studies, including this one from the University of Texas, have refuted the thesis.
That study, published July 2, 2014, in the Annals of Pharmacotherapy,  found that Testosterone therapy was heart-protective even for individuals with increased cardiac risk factors.
found that Testosterone therapy was heart-protective even for individuals with increased cardiac risk factors.
As reported in WebMD, “men at greater risk for heart problems who used testosterone had a lower rate of heart attacks than similar men who did not receive this treatment, the researchers said.”
This Harvard Medical School article points out that men with the lowest Testosterone have higher cholesterol levels, a risk factor for heart disease.
No one is saying that Testosterone does not have risks.
Everything has risks, even exercise.
This does not mean exercise is dangerous for you.
The key is moderation and educating yourself.
Another indicator that the deck was stacked against Testosterone therapy comes from an article written by journalist Dennis Thompson.
According to the article, the FDA review pointed out there’s no clear scientific evidence showing Testosterone replacement can reverse some of the effects of aging.
The “Low-T” craze is aided by consumer advertising for remedies that promise renewed vitality and strength for aging men.
It also noted that there’s growing evidence many men who are receiving Testosterone Replacement Therapy do not need it.
The last sentence is correct.
 Young bodybuilders, for example, don’t need to take Testosterone supplements for health reasons.
Young bodybuilders, for example, don’t need to take Testosterone supplements for health reasons.
However, it is flat out wrong to say there is “no clear scientific evidence showing testosterone replacement can reverse some of the effects of aging.”
You can raise valid questions about the safety of Testosterone, but please don't say with a straight face that it doesn't work.
It's like claims made years ago that anabolic steroids should be banned because they didn’t work.
In the same article, the writer quotes a University of Washington endocrinologist, who said, “There’s a large group of men out there who are getting older, and they are looking for ways to evade the consequences of aging.”
The word “evade” is telling.
In tax law, tax avoidance is permitted.
Tax evasion is not.
The clear implication of this statement is that men who would like to put off the symptoms of aging are illegitimately “evading” the natural order of things.
Let's see what that endocrinologist (who is not yet in his 50's) says when his Testosterone levels drop.
He might change his mind about age “evasion.”
The Final Word
 There’s a battle underway in the scientific community concerning the benefits of longer life.
There’s a battle underway in the scientific community concerning the benefits of longer life.
Everyone knows living longer is preferable to the alternative of early death. Still, considering life extension technologies are just now becoming available, we just don’t yet know what the long-term implications are of people living at 80 the way they did at 50.
Furthermore, as in the case of Testosterone products, regulatory bureaucracy seems to set up against what could be useful life extension technologies.
In the years ahead, not only will society have to reach a scientific consensus on the implications of longer life, but political attitudes will need to change as well.
Contact us for a FREE, no-obligation discussion of the benefits of testosterone.
Reference
Testosterone and Cardiovascular Disease.
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- LabCorp Announces a Change to the Testosterone Reference Range [Last Updated On: April 16th, 2025] [Originally Added On: June 23rd, 2019]
- Important Facts About Testosterone Therapy Before Buying [Last Updated On: April 18th, 2025] [Originally Added On: July 13th, 2019]
- Soy: Does it Lower Testosterone? [Last Updated On: October 18th, 2024] [Originally Added On: August 30th, 2020]
- Testosterone Treatments May Successfully Reverse Type-2 Diabetes in Some Men [Last Updated On: April 15th, 2025] [Originally Added On: November 13th, 2020]
- Testosterone Replacement Therapy (TRT) May Prevent Heart Attacks and Diabetes [Last Updated On: April 21st, 2025] [Originally Added On: November 17th, 2020]
- Did You Know? Recent Studies Have Confirmed the Link Between Low Testosterone (“Low-T”) and Depression. [Last Updated On: April 17th, 2025] [Originally Added On: January 10th, 2021]
- New Study Finds Testosterone Does Not Increase Your Heart Attack Risk [Last Updated On: April 14th, 2025] [Originally Added On: January 11th, 2021]
- The Great Testosterone Debate [Last Updated On: April 20th, 2025] [Originally Added On: January 14th, 2021]
- Testosterone Replacement Therapy Lowers Heart Attack Risk [Last Updated On: April 19th, 2025] [Originally Added On: January 18th, 2021]
- New Study Says: The Benefits of Testosterone Replacement Therapy Outweigh The Risks [Last Updated On: April 22nd, 2025] [Originally Added On: January 19th, 2021]
- Male Menopause. Fact or Fiction ? [Last Updated On: April 23rd, 2025] [Originally Added On: January 20th, 2021]
- Testosterone: How Much Do You Really Know About This Masculine Hormone? [Last Updated On: October 6th, 2024] [Originally Added On: February 9th, 2021]
- Low-T: What are healthy levels of Testosterone and why is it difficult to measure? [Last Updated On: September 11th, 2025] [Originally Added On: April 3rd, 2021]
- Testosterone Therapy May Be Good for the Heart if You Have Low-T [Last Updated On: May 3rd, 2025] [Originally Added On: July 21st, 2021]
- A Recent Study Concludes: Testosterone DOES NOT Cause Prostate Cancer [Last Updated On: September 14th, 2025] [Originally Added On: August 16th, 2021]
- In the Battle Against Aging, When do the Risks Outweigh the Rewards? [Last Updated On: April 4th, 2025] [Originally Added On: August 18th, 2021]
- New Study Concludes: Boosting Testosterone Levels Lowers Men's Death Risk [Last Updated On: May 11th, 2025] [Originally Added On: August 20th, 2021]
- Testosterone Replacement Therapy Slows Prostate Cancer! [Last Updated On: April 2nd, 2025] [Originally Added On: September 13th, 2021]
- Research proves that Testosterone Therapy Boosts Fertility! [Last Updated On: April 5th, 2025] [Originally Added On: September 26th, 2021]
- Free Testosterone and Sex Hormone-Binding Globulin [Last Updated On: April 6th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Women [Last Updated On: April 8th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Metabolic Syndrome [Last Updated On: April 3rd, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Disease Prevention [Last Updated On: March 31st, 2025] [Originally Added On: October 15th, 2021]
- Judge Vacates $140 Million Verdict in Testosterone Lawsuit [Last Updated On: April 1st, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Estrogen [Last Updated On: April 9th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone and Aging [Last Updated On: April 10th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone Replacement Therapy (TRT) Benefits [Last Updated On: April 11th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone and Male Menopause [Last Updated On: March 30th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone Battles Obesity [Last Updated On: March 29th, 2025] [Originally Added On: October 16th, 2021]
- Why You Need Testosterone Replacement Therapy [Last Updated On: May 14th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone FAQ's [Last Updated On: May 13th, 2025] [Originally Added On: October 25th, 2021]
- How Testosterone Impacts Sexual Preferences In Men and Women [Last Updated On: March 28th, 2025] [Originally Added On: October 30th, 2021]
- Growth Hormone and The Thyroid Gland [Last Updated On: April 24th, 2025] [Originally Added On: November 19th, 2021]
- How Does Masturbation Affect Testosterone Levels? Exploring the Science [Last Updated On: May 24th, 2025] [Originally Added On: March 27th, 2022]
- Testosterone Therapy Increasingly Used to Help Men Take Control of Aging [Last Updated On: May 25th, 2025] [Originally Added On: May 30th, 2022]
- The many benefits of Testosterone Replacement Therapy (TRT) [Last Updated On: November 1st, 2025] [Originally Added On: June 13th, 2022]
- Tlando Testosterone - A Brand New Way to Treat Low-T Safely with a Testosterone Pill [Last Updated On: May 28th, 2025] [Originally Added On: July 12th, 2022]
- Safe Tlando Testosterone Changes Landscape of Low-T Therapy [Last Updated On: May 30th, 2025] [Originally Added On: August 15th, 2022]
- Systems to Monitor Testosterone Replacement Therapy (TRT) [Last Updated On: October 12th, 2025] [Originally Added On: September 21st, 2022]
- Testosterone May Help You Keep Your Job (Or Find Another) [Last Updated On: June 12th, 2025] [Originally Added On: October 4th, 2022]
- Toxic Chemicals are Killing your testosterone…And your Manhood! [Last Updated On: October 28th, 2024] [Originally Added On: October 10th, 2022]
- A new study reveals that Testosterone improves body composition in men with low testosterone! [Last Updated On: October 22nd, 2025] [Originally Added On: October 17th, 2022]
- A former Mr. Olympia speaks about testosterone [Last Updated On: October 10th, 2025] [Originally Added On: November 8th, 2022]
- Testosterone Blockers Thwart Melanoma [Last Updated On: June 9th, 2025] [Originally Added On: December 11th, 2022]